Two physicians who are leading the charge on early at-home COVID-19 treatment to reduce hospitalization and death, become infected with the virus and are now recovering after following the regiment they have preached.
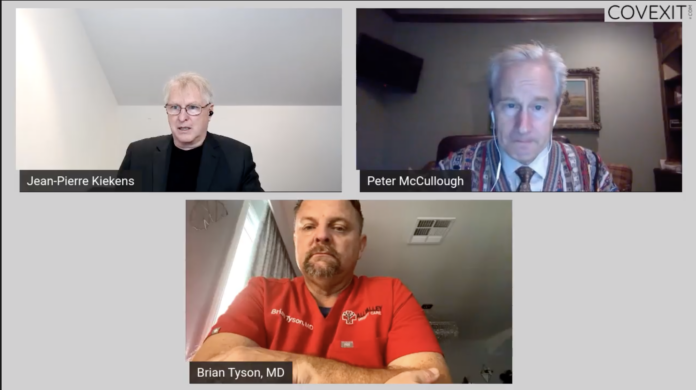
The surprise announcement of their illnesses came during an October 27 webcast by Covexit.com. Peter McCullough, M.D., a public health expert, researcher and cardiologist at the Baylor Heart and Vascular Institute in Dallas, Texas, was scheduled to discuss the COVID treatment algorithm he helped design and was published August 7 in the American Journal of Medicine. During the presentation, McCullough revealed he was currently sick with the virus and is following his own protocol.
“I fully expect to have a prompt recovery, to return to work, and avoid the risk of hospitalization and death,” said McCullough.
McCullough demonstrated his recovery, one week later in a video.
Moderator Jean-Pierre Kiekens then brought in another champion of early at-home treatment to the discussion, Brian Tyson, M.D., a family physician in California. Tyson said, he too, tested positive with the virus and felt remarkably better after two days of the at-home regimen.
Physicians Avoiding the Hospital
McCullough said he tested positive the day before his presentation but showed symptoms several days earlier. The day before his test result came back, McCullough said he began treatment for his particular cohort in the algorithm, a patient over age 50 and with two or more pre-existing conditions (asthma, heart disease).
McCullough’s home regimen consists of the anti-viral drug, Ivermectin (IVM), the antibiotic, Azithromycin, zinc, vitamin D, an increase in his daily dose of aspirin for mild heart disease, and plenty of fresh air to avoid re-inoculation. If his symptoms don’t improve in 5 days, McCullough says he will start taking prednisone.
Tyson said he also used IVM in his treatment and noticed a huge improvement in symptoms on day two. “It is still lingering a little, bit. It’s more like a head cold, but the IVM seemed to really knock it out,” said Tyson.
The IVM and the antibiotic are “off label” use, meaning, they have been approved for other illnesses, not for COVID-19. Both physicians looked well, but tired, and McCullough sneezed a few times and sounded congested. McCullough said he ran six miles, four days earlier.
The Case for Early Treatment
The webcast was devoted primarily to McCullough’s research on early, at-home COVID-19 treatment. The virus shows no sign of dissipating, says McCullough, and this is the one approach the U.S. has not pushed. “If we don’t take a more comprehensive approach, our hospitals will become overwhelmed, the mortality rate can be incredibly high and this is, in fact, bearing out,” said McCullough
Unlike the flu or viruses that caused previous pandemics, the Sars-CoV2 virus (the virus that causes COVID-19) can lead to three distinct, lethal outcomes: viral damage to organs, cytokine storm, and micro-thrombosis (blood clots). “The mortality curve can go out 30 days,” said McCullough
There are four pillars to controlling a pandemic, stated McCullough, but the media and public health authorities focus on only three of them, with Dr. Anthony Fauci’s presentation on the Yale Global Health Network October 26, being a case in point. “The entire message was contagion control, shelter in place, and wait for a vaccine. There was no mention of early home treatment.” Incidentally, Fauci’s presentation on Zoom was standing room only, McCullough’s presentation had 57 participants.
People are going to get sick with COVID-19 if they haven’t already, said McCullough. “Early home treatment can be the only method for reducing hospitalizations and death once an individual gets sick. The hospital should only be a safety net for survival. It should not be the first place of treatment” said McCullough. McCullough says the U.S. should follow what India and Brazil have done and make available at-home COVID-19 treatment kits.
The average patient gets to the hospital about 14 days after the onset of illness, said McCullough after the more-deadly complications start presenting. McCullough and colleagues released a meta-analysis of over 5,700 patients, that showed early COVID could reduce mortality by 24 percent.
Traditional Approvals
McCullough and Tyson said in an emergency, such as there is with the COVID pandemic, there is no time for traditional treatment approval. “We just don’t have 20 years,” said McCullough.
Because the early treatment approach with antivirals, including hydroxychloroquine (HCQ), has yet to receive the green light from the U.S. Food and Drug Administration (FDA) for COVID, physicians have been reluctant to use it. States have restricted off label anti-viral drug dispensing, for example, and physicians and pharmacists fear the loss of their license. Additionally, the FDA is stockpiling HCQ after removing emergency use authorization for the drug in June to treat COVID-19.
“We are not used to the pandemic model,” said Tyson, who started treating COVID patients at home, early starting in March. “We are so based on protocol and evidence-based medicine but with a pandemic, there is no information. You just have to basically figure it out.”
Both physicians say early at-home treatment does not mean COVID-10 should be treated less seriously. “It is a very serious disease and can progress to deadly levels with no explanation. The idea of not treating it until a patient gets to the hospital does not make sense,” said Tyson.
Telemedicine, home oxygen, and at-home devices to help measure vitals such as oxygen levels in the blood can make even more of a case for early at-home treatment, said McCullough and Tyson. Tyson said x-rays too are an important component and can be done on an outpatient basis.
“Medicine is both an art and a science. In this pandemic, we have focused on the science, in randomized trials, in new drug development, and the body count has been through the roof, “ said McCullough. [What is needed is] clinical judgment, careful observation, being able to quickly adapt to new concepts.”
“I think so many lives can be saved, that is why we are putting every bit of our professional and personal effort in this message of early home treatment for COVID-19,’ said McCullough. “We know what to do, we just treat too late.”
AnneMarie Schieber (amschieber@heartland.org) is managing editor of Health Care News.
Internet info:
“Outpatient Early Treatment Algorithm for COVID-19 – A Webinar with Peter A. McCullough, M.D., MPH, October 27, Covexit.com: https://www.minds.com/newsfeed/1167874917079040000




















[…] Doctors with COVID-19 Put Early At-Home Treatment to the Test […]
[…] Doctors with COVID-19 Put Early At-Home Treatment to the Test […]
One lesson in all of this is for patients to find independent primary care physicians, if they can. The majority now employed by hospitals or medical systems, will be much less free to prescribe off label, no matter the wishes of their state. AAPS is in the process of compiling a list of doctors who will provide early Covid-19 treatment.
That is an interesting observation, the connection between physicians and the hospitals that employ them. If the goal of health care is to drive resources to one particular industry, failing to treat an illness before it becomes an expensive mess, would be in line with that.
[…] Doctors with COVID-19 Put Early At-Home Treatment to the Test. […]
[…] the globe promoting his published protocol in The American Journal of Medicine, August 7, 2020. McCullough, himself is being treated under the protocol after he tested positive for COVID-19 on October […]