If you are old enough, you remember Grandma telling you to play outside and get fresh air and sunshine. Fresh air dilutes and dries out germs, and the ultraviolet light in sunshine kills them.
We now see this advice in technical jargon in the respected American Journal of Medicine, (see “New Treatment Protocol,” page 6).
“It is well recognized that COVID-19 exists outside the human body in a bioaerosol of airborne particles and droplets. Since exhaled air in an infected person is considered to be ‘loaded’ with inoculum, each exhalation and inhalation is effectively re-inoculation,” states lead author Peter McCullough, M.D., M.P.H. “We propose that fresh air could reduce re-inoculation and potentially reduce the severity of illness and possibly reduce household spread during the quarantine. This calls for open windows, fans for aeration, or spending long periods of time outdoors away from others with no face-covering in order to disperse and not re-inhale the viral bio-aerosol.”
Masks: More Harm than Good?
Patients who were nursed outdoors during the 1918 influenza pandemic fared better. Personal protective equipment (PPE), including proper masks, is, of course, important when caring for infected patients. A 2015 study, however, showed that medical personnel required to wear a cloth mask throughout their shift had a 13-fold higher risk of influenza-like illness than those wearing a medical mask and a nearly 7-fold higher risk than controls using “standard practice,” which might or might not involve continuous mask-wearing.
The air inside the mask is definitely stale, and likely violates OSHA (U.S. Occupational Safety and Health Administration) standards for workplace ventilation. Masks I tested, including surgical masks, a KN95 mask, and some cloth masks, had a carbon dioxide level greater than 10,000 ppm (parts per million). The OSHA limit is 5,000 ppm. Levels this high can cause drowsiness or headache, and the majority of medical workers complain of headaches when constantly masked.
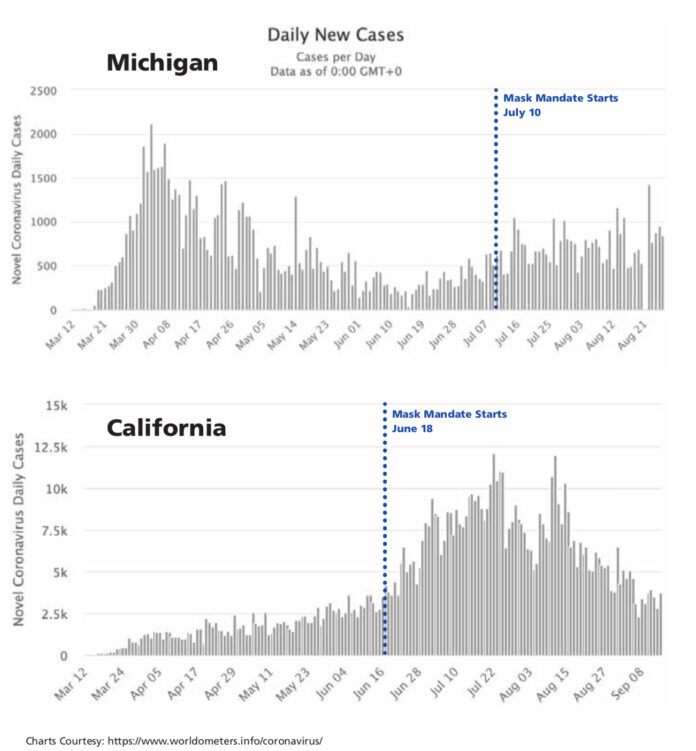
Can we defeat COVID-19 in eight weeks if everyone is masked? This is the opinion of CDC director Robert Redfield, M.D., based on a study in a Massachusetts hospital system and a report of two hairstylists who did not infect customers. This falls far short, however, of evidence that would justify deploying mask police against the whole population. In fact, during a mask mandate in California, infection rates rose (see figures, this page).
The potential harm from universal mask mandates, versus hypothetical (and small) benefits, is apparently not considered by authorities imposing the mask edicts.
Jane Orient, M.D. is executive director of the Association of American Physicians and Surgeons (AAPS) and a policy advisor to The Heartland Institute.
Internet info:
Marilyn M. Singleton, M.D., J.D., “Mask Facts,” Association of American Physicians and Surgeons, June 1, 2020: https://aapsonline.org/mask-facts/