Editor’s note: Below is an article that was posted on The Heartland Institute blog on September 23, 2021, by James Agresti, the president of Just Facts and a policy advisor to The Heartland Institute. The article lists an extensive list of studies and data regarding mask effectiveness in controlling the spread of COVID -19 and for that reason, Health Care News is presenting the text in its entirety.
By James Agresti
In a terse essay titled “Science and Dictatorship,” Albert Einstein warned that “Science can flourish only in an atmosphere of free speech.” And on his deathbed, Einstein cautioned, “Whoever is careless with the truth in small matters cannot be trusted in important affairs.”

With reckless disregard for both of those principles, powerful government officials and big tech executives have corrupted or suppressed the central scientific facts about face masks. The impacts of this extend far beyond the issue of masks and have caused widespread harm and countless deaths.
Despite the fog of contradictory claims and changing government guidelines, dozens of scientific journals have published consistent data that establish these facts:
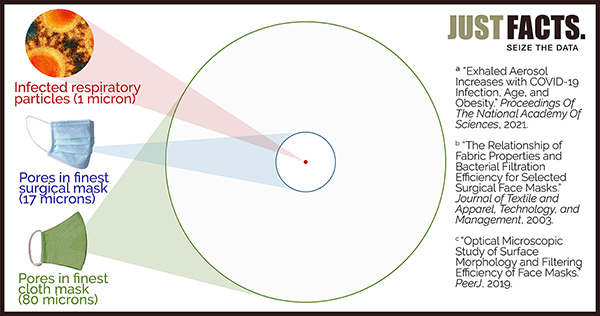
- Covid-19 is mainly spread by microscopic aerosols generated by breathing, talking, sneezing, and coughing. The vast bulk of these infectious aerosols easily penetrate common masks because 90% of the aerosols are less than 1/17th the size of pores in the finest surgical masks and less than 1/80th the size of pores in the finest cloth masks.
- Aerosols are light enough to stay airborne for minutes or hours, and hence, they also travel freely through gaps around the edges of the cloth and surgical masks.
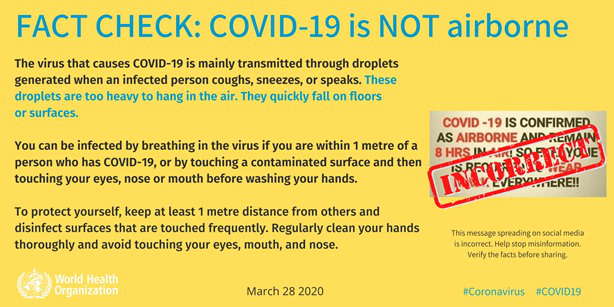
- Governments enacted mask mandates based on the false assumption that C-19 is mainly transmitted by large droplets generated by coughing, sneezing, and spittle. These droplets are bigger than the pore sizes of most masks and only remain airborne for a few seconds after they are emitted.
- For more than a year, the World Health Organization and the U.S. Centers for Disease Control and Prevention denied and downplayed the threat of aerosol transmission while issuing guidelines that don’t amply prevent it. This enabled C-19 to decimate the most vulnerable members of society, like those in hospitals and nursing homes.
- The CDC and WHO quietly admitted in the spring of 2021 that aerosols pose a major threat of transmission but have still not adequately updated their guidelines to reflect this reality. This has allowed countless preventable deaths to continue.
- The risk of aerosol transmission can be greatly reduced by disinfecting air with ultraviolet (UV) light, which is part of the energy spectrum emitted by the sun. This simple and safe technology neutralizes airborne microbes and has been successfully used to control the spread of contagious respiratory diseases for more than 80 years.
- Randomized controlled trials—which are the “gold standard” for clinical research—have repeatedly measured the effects of masks on preventing the spread of contagious respiratory diseases. These trials have found inconsistent benefits from N95 masks in healthcare settings and no statistically significant benefits from any type of mask in community settings.
- The only randomized controlled trial that evaluated cloth masks found that mandating them causes significant disease transmission in high-risk healthcare settings.
- Observational studies—which are a weaker form of evidence than randomized controlled trials—find that masking schoolchildren provides negligible or no benefits.
- Lab studies—which are the weakest form of clinical evidence—don’t support the notion that surgical or cloth masks reduce the transmission of Covid-19.
- Masks of all types have negative impacts on some people, including headaches, difficulty breathing, increased cardio-pulmonary stress during exercise, marked discomfort, and weakened social bonds.
- Because humans create carbon dioxide as they breathe, the CO2 concentration of the air they exhale is about 100 times higher than in fresh air. Masks restrict airflow and thus cause the wearers to rebreathe some of the air they exhale.
- The average CO2 concentrations inhaled by people wearing N95 masks range from 2.6 to 7.0 times OSHA’s work shift limit for CO2. These levels cause headaches and chest pains in some people.
- The average CO2 concentrations inhaled by people wearing cloth and surgical masks range from 2 to 3 times the government CO2 limits for classrooms in many countries. These levels may impair certain high-level brain functions like initiative, strategic thinking, and complex decision-making.
The leaders of big tech corporations like Facebook, Twitter, and Google/YouTube have empowered government officials who misled the public about every matter above and others. Together, they continue to do so by engaging in actions that resemble common disinformation tactics. These include but are not limited to cherry-picking, censorship, muddying the waters, citation bluffs, non-sequiturs, half-truths, and outright falsehoods.
A very common and naive talking point about masks is that “experts say” they reduce the spread of Covid-19. Such statements are oblivious to the reality that other experts disagree with that opinion, like these for example:
- Dr. Erica Shenoy, the Associate Chief of the Infection Control Unit at Massachusetts General Hospital, along with four other medical professionals, wrote in the New England Journal of Medicine that “wearing a mask outside health care facilities offers little if any, protection from infection.”
- Dr. Martin Kulldorff, a Professor of Medicine at Harvard Medical School, has stated, “Children should not wear face masks” because “they don’t need it for their own protection and they don’t need it for protecting other people either.”
- Tamara van Ark, a public minister in The Netherlands, announced the conclusion of the nation’s National Institute for Health as follows: “Because from a medical perspective there is no proven effectiveness of masks, the Cabinet has decided that there will be no national obligation for wearing non-medical masks.”
- Dr. Joseph Allen, an associate professor and the director of the Healthy Buildings program at Harvard University, wrote, “The truth is, for kids, Covid-19 is like the flu, and we don’t make kids wear masks in school for that.”
- Dr. Shamez Ladhani, a professor of pediatric infectious diseases and vaccinology at St. George’s University of London, wrote that masking may help reduce Covid-19 transmission when used with other “infection control measures, but I have yet to see any convincing evidence that masking in and of itself significantly contributes to reducing infection and transmission” in schools and other institutional settings.
- Dr. Jay Bhattacharya, a Professor of Medicine at Stanford University, said, “On net, I think the masks not only have not been effective but have been harmful.”
- Dr. Lisa Brosseau and Dr. Margaret Sietsema, researchers specializing in infectious diseases and respiratory protection, wrote, “There is no scientific evidence” that “cloth or surgical masks” are “are effective in reducing the risk of SARS-CoV-2 transmission.”
Regardless of what any experts say or how many say it, their opinions do not constitute scientific facts. Yet, journalists, commentators, and “fact-checkers“ often treat the mere opinions of selected experts as “facts” or “science,” and politicians use the phrase, “science says“ as if it magically turns claims into facts.
Such misuse of the word “science” has been a longstanding problem. As the renowned physicist Richard Feynman remarked half a century ago, “When someone says, ‘Science teaches such and such,’ he is using the word incorrectly.” People who are actually discussing science, explained Feynman, don’t “say science has shown”—but rather “this experiment, this effect, has shown.”
This article presents actual science, and there is no substitute for it when lives are on the line. Although greatly condensed from more than 500 hours of research, these thoroughly vetted facts will take more than an hour for most people to read. This is the price of being informed instead of indoctrinated.
Because masks have been used in operating rooms for more than a century, many studies have been conducted on them dating back to at least 1935. One might assume that these studies quickly found benefits given that the main purpose of surgical masks is simple: to prevent bacteria from the mouths and noses of surgeons from falling into the open wounds of their patients.
Yet more than half a century later, a 2001 paper in the Journal of Hospital Infection reviewed all known studies about “surgical face masks in the operating theatre” and found that their “effectiveness remains unresolved.” A 2016 paper found the same. Such outcomes commonly occur when the effects of something are very minimal or difficult to measure.
Measuring the impact of masks on the spread of infectious diseases in homes and public places is considerably harder than in operating rooms. This is because such settings are far more diverse and less controlled than operating rooms, which are subject to strict infection control protocols.
These facts suggest that cocksure and simple-minded statements like “masks work” should be treated with skepticism.
In 2019—the year before Covid-19 pandemic began—the World Health Organization published a lengthy analysis of different strategies to limit the impact of the flu in “community” or “non-healthcare“ settings. The analysis found “there was no evidence that face masks are effective in reducing transmission” of the flu in these situations.
Covid-19 differs from the flu, and one of the main differences is that C-19 is much more transmissible. This raises the question: How can masking reduce the community spread of C-19 when there is “no evidence” that it does so for the flu?
Fortunately, a vital tool to answer that question is provided in WHO’s supplement to the same analysis. In it, WHO correctly notes that the key to sorting out masses of studies is to rank the “quality of evidence” from strongest-to-weakest in the following order:
- Randomized controlled trials (RCTs): These are studies in which people are randomly assigned to receive or not receive a certain treatment. Done properly, these are the “gold standard“ for clinical research because they provide “a rigorous tool to examine cause-effect,” which “is not possible with any other study design.” That is why the medical textbook Rutherford’s Vascular Surgery calls RCTs “the pinnacle in clinical design.”
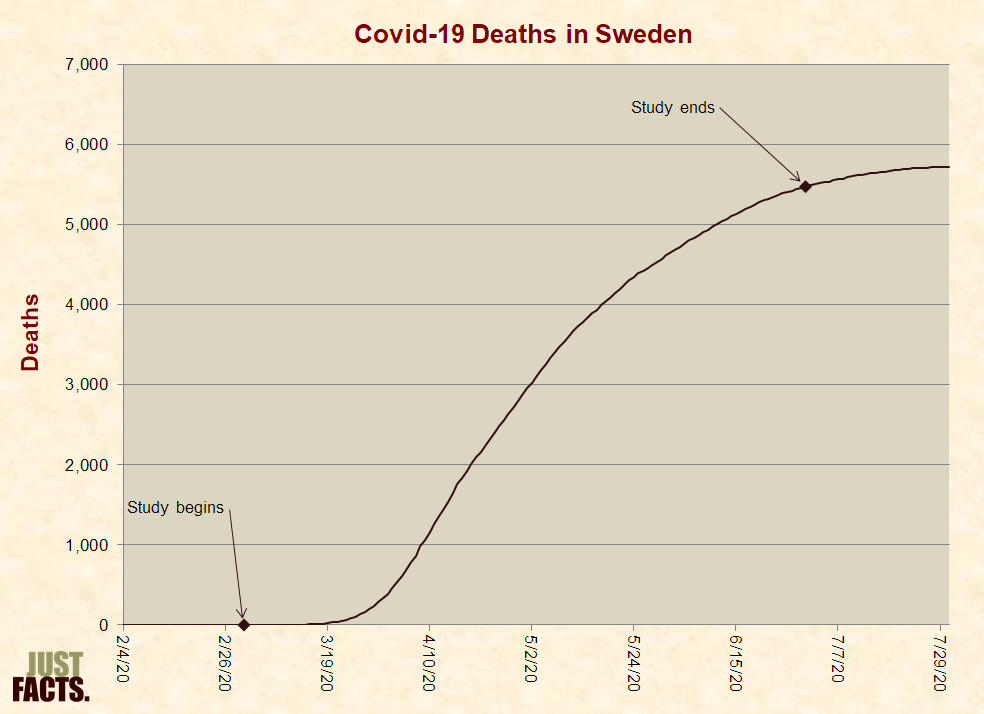
- Observational studies: These studies observe the outcomes of people who have not been randomly assigned a certain treatment. Unless their results are mathematically and logically overwhelming, observational studies can “rarely” determine the effects of a treatment because a host of other factors are always at play when it comes to people’s health. For example, measuring the C-19 death rates of nations with and without mask mandates cannot determine the effects of the mandates because many factors impact C-19 death rates. As documented in a 2018 paper in the European Heart Journal, “it is not possible to make reliable therapeutic inferences from” observational studies.
- Laboratory and simulation studies. These are experiments conducted under artificial conditions and are typically the weakest form of clinical evidence. As explained by the UK’s Department of Health, such “studies provide only theoretical evidence” because they “are run in controlled environments that may not accurately reflect the behaviours that we observe in real life.” Likewise, a 2020 paper in a German medical journal explains that such studies can “provide important mechanistic insights” about Covid-19 transmission, but they “never approximate real-world conditions,” and thus, they should “not directly inform policy decisions.”
The quality gaps between those types of studies are so great that WHO adopted a “general principle” to “not review simulation studies” if observational studies were available and to “not review observational studies or simulation studies” if RCTs were available.
However, WHO broke that rule for masks while explaining that even though all “ten RCTs” showed “no evidence that face masks are effective in reducing transmission” of the flu, “there is mechanistic plausibility for the potential effectiveness of this measure.” Thus, WHO flouted its own principle and “conditionally recommended” that asymptomatic people wear face masks “in severe epidemics or pandemics, to reduce transmission in the community.”
Relevance
Beyond the general quality of a study, another important factor to consider is how applicable it is to the issue at hand. Studies on trained nurses who wear N95 masks to reduce the spread of tuberculosis during 10-minute interactions in sanitized hospital wards are less relevant to the present issue than studies on 5-year-olds wearing cloth masks for six hours in poorly ventilated schoolrooms during the C-19 pandemic.
Of great import for understanding the coming facts, the three main types of masks from the highest-to-lowest quality are:
- N95 masks or respirators, which are mainly intended to prevent wearers from inhaling fine aerosols and microscopic particles. These are supposed to be used only once, must meet strict filtration standards, and must be moldable to each user’s face to form a tight seal. Because N95s heavily restrict breathing and “may place a burden on an employee’s health,” OSHA requires employers to conduct a medical evaluation of each employee who wears them.
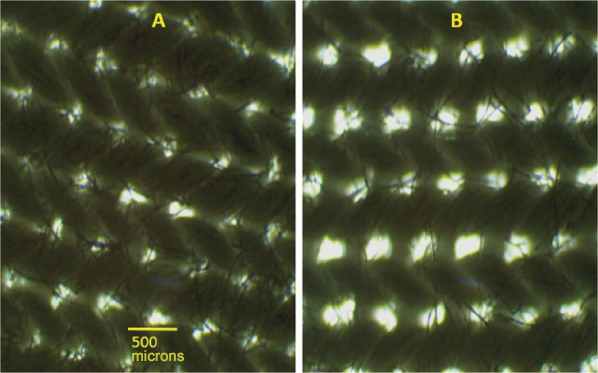
- Surgical or medical masks, which are primarily designed to prevent wearers from spraying liquid droplets and large particles on other people. The FDA’s Covid-19 guidance for these masks states that they cannot be labeled “for antimicrobial or antiviral protection” and cannot make “filtration claims” for particles of any size. Per a 2013 paper in the Journal of Occupational and Environmental Hygiene, surgical masks have “poor filtration” and a “poor fit,” and thus, they “cannot be expected to significantly reduce the inhalation of infectious aerosols.” They are supposed to be used only once.
- Cloth masks, which are made of common fabrics that tend to be highly permeable. These masks were already worn before the C-19 pandemic in developing countries because they are inexpensive and can be used more than once. The CDC says they should be washed at least once a day, and washing them makes the fabrics even more permeable.
In July 2020, the Journal of the American Medical Association published a commentary titled “Universal Masking to Prevent SARS-CoV-2 Transmission—The Time Is Now.” The authors—all of whom were CDC employees—argued that the benefits of using masks during surgery are relevant to the general public. This leap of logic conflates surgical masks with cloth masks, sterilized operating rooms with subways, and open wounds with people’s faces.
The authors also claimed—without citing any research—that it would be “absurd” to conduct surgery without masks “because it is known that use of face coverings under these circumstances reduces the risk of surgical site infection caused by microbes generated during the surgical team’s conversations or breathing.”
That assertion is at direct odds with the strongest, most relevant research on this issue. This was summarized in a 2016 paper published by “the leading journal and database for systematic reviews in health care.” After conducting an extensive search for all available RCTs on the use of surgical masks to prevent wound infections, the authors located three trials and found “there was no statistically significant difference in infection rates between the masked and unmasked group in any of the trials.”
This straightforward example dramatically illustrates how the claims of “experts” published in one of the world’s leading medical journals can be at odds with documented facts. Yet with callous disregard for the facts—and thus the wellbeing of people—Google/YouTube, Facebook, and Twitter have banned factual statements about masks that conflict with the opinion of their chosen experts.
Like the 2019 analysis of RCTs by the World Health Organization, other comprehensive analyses of gold-standard studies have found no evidence that low-quality masks reduce the spread of the flu in community settings. Moreover, such studies have found limited evidence that any type of mask protects against the flu in any setting:
- In 2010, the journal Epidemiology & Infection published a “systematic review” of studies that examined the use of “face masks to prevent transmission of influenza virus,” including several RCTs. The analysis found that “while there is some experimental evidence that masks should be able to reduce infectiousness under controlled [i.e., lab] conditions, there is less evidence on whether this translates to effectiveness in natural settings” and “little evidence to support the effectiveness of face masks to reduce the risk of infection.”
- In 2011, the journal Influenza and Other Respiratory Viruses published a “systematic review of the scientific evidence” on the “use of masks and respirators to prevent transmission of influenza.” The authors examined eight RCTs and found:
- that “none of the studies we reviewed established a conclusive relationship between mask/respirator use and protection against influenza infection.”
- “there is a limited evidence base to support the use of masks and/or respirators in healthcare or community settings.”
- “some useful clues” that “correct and consistent wearing of masks/respirators may improve their effectiveness,” but “this remains a major challenge” in “the context of a formal study and in everyday practice.”
- In May 2020, a CDC journal named Emerging Infectious Diseases published a “systematic review” of 10 RCTs that “reported estimates of the effectiveness of face masks in reducing” the spread of the flu in community settings. A “pooled analysis” of their results found “no significant reduction in influenza transmission with the use of face masks,” regardless of whether they are “worn by the infected person” to protect others, or if they are worn by “uninfected persons” to protect themselves from people who are infected.
All of those flu RCTs are highly relevant to Covid-19 because:
- both diseases are transmitted by RNA viruses that produce respiratory tract infections.
- more than 87% of virus-laden respiratory particles exhaled by people with either disease are less than 1 micron in diameter. These can easily penetrate surgical and cloth masks because the average pore sizes of:
Broadening the research beyond the flu to other types of infectious respiratory diseases, RCTs have found inconsistent evidence that higher-quality masks may help in healthcare settings but no statistically significant evidence that any type of mask helps in community settings:
- In 2017, the journal Clinical Infectious Diseases published “a systematic review and meta-analysis” about the “effectiveness of masks and respirators against respiratory infections in healthcare workers.” It found that RCTs “indicated a protective effect” from masks but that the “evidence is sparse and findings are inconsistent within and across studies.” It also found that “N95 respirators conferred superior protection” to lower-quality masks.
- In March 2020, the Journal of Evidence-Based Medicine published a systematic review of six RCTs on masks published in the past five years. It found “there were no statistically significant differences in preventing laboratory-confirmed influenza, laboratory-confirmed respiratory viral infections, laboratory-confirmed respiratory infection and influenza-like illness using N95 respirators and surgical masks.” It only compared these masks to one another and not to using no masks.
- In June 2020, the Annals of Internal Medicine published a “living rapid review” of mask studies involving viral respiratory infections. The review found:
-
- 8 RCTs in household settings showed “surgical masks were not associated with decreased risk” for respiratory disease regardless of whether masks were worn by sick people, other people in their households, or everyone.
- 2 RCTs in college dorms showed “no significant differences between a surgical mask versus no mask and risk for influenza-like illness.”
- 2 RCTs among pilgrims to Mecca that showed surgical masks “were not associated with decreased risk for infections,” even when healthy and sick people lived in the same tents.
- In April 2021, the authors of the above living review updated their research a fifth time to incorporate all newly published mask studies. Only one of these was an RCT, and it found that wearing a surgical mask in community settings was associated with a “small” and statistically insignificant reduction in the odds of catching C-19. More precisely, the study found with 95% confidence that people assigned to wear surgical masks in Denmark had “a 46% reduction to a 23% increase” in C-19 infections compared to those who were assigned to not wear a mask. Of special import to the next analysis below, each mask wearer was given “a supply of 50 surgical masks” and “instructed to change the mask if outside the home for more than 8 hours.”
- In July 2020, the Center for Evidence-Based Medicine at Oxford University published an analysis of 12 RCTs on masks. It found that:
- “masks alone have no significant effect in interrupting the spread” of the flu or flu-like illnesses “in the general population, nor in healthcare workers.”
- one of the largest RCTs—which studied 1,607 healthcare workers in 74 “high-risk wards” of 14 Vietnamese hospitals—showed that people assigned to wear cloth masks were about 13 times more likely to contract a respiratory infection than those who wore surgical masks.
The last of those studies are particularly relevant to C-19 mask mandates because:
- it is the only RCT that evaluated cloth masks, the most commonly worn mask during the C-19 pandemic.
- 85% of all laboratory-confirmed infections in the study were rhinoviruses, which share a key trait with C-19: both can be transmitted by fine particles (called aerosols) that easily penetrate cloth masks.
- the workers who were assigned to wear cloth masks got infected at 3.49 times the rate of workers who were told to “continue with their normal practices, which may or may not have included” wearing cloth or surgical masks. Though “almost all” of these workers wore some type of mask at certain times, only 24% of them wore a mask for more than 70% of their working hours. In other words, the people mandated to wear cloth masks were 3.5 times as likely to become infected than those who wore masks occasionally.
When the RCT on cloth masks was published in 2015, the lead author of the study, Raina MacIntyre of the University of New South Wales (Australia)—stressed: “it is important for global disease control that the use of cloth masks be discouraged in high-risk situations.” However, she and some of her coauthors began backpedaling five years later in 2020 when governments began mandating masks for C-19. MacIntyre and company did this by:
- Claiming without evidence that “the physical barrier provided by a cloth mask may afford some protection”—despite the results of their own paper which:
- found via laboratory testing that particle “filtration was extremely poor (almost 0%) for the cloth masks.”
- “caution against the use of cloth masks.”
- Claiming in a 2020 paper in the International Journal of Nursing Studies that eight RCTs showed community masking “appeared to be effective,” even though:
- a May 2020 paper in the CDC journal Emerging Infectious Diseases examined the very same RCTs (plus two others) and found “no significant reduction in influenza transmission with the use of face masks” in a “pooled analysis.”
- Not one of the eight RCTs they cited found a statistically significant positive impact from masking.
The last of those papers—which was coauthored by MacIntyre and published by the CDC—buries the results of the RCT two-thirds of the way into a lengthy paragraph. There, the authors reveal that the “intent-to-treat analysis”—which is the actual RCT—“showed no significant difference” in outcomes between the people who were assigned to wear masks and not wear masks.
While concealing the gold standard results of their own study, MacIntyre’s team focused their analysis on a subset of people who had the highest “adherence to mask use.” This violates the very essence of RCTs, which are supposed to be “randomized control trials.” Randomization is the linchpin that allows these studies to determine cause and effect.
For that reason and others, Dr. Alyson Haslam of the Oklahoma State University Center for Health Sciences Research publicly criticized MacIntyre and her colleague (Dr. Abrar Ahmad Chughtai) for spreading “incorrect/biased summaries of published articles.”
MacIntyre and Chughtai replied without confronting the central fact of this matter: people who were more diligent about wearing masks may have taken other precautions to avoid getting sick, like social distancing or washing their hands more often. In other words, their conclusion that masks “appeared to be effective” is not based on RCTs, even though their paper claims to be an analysis of “randomised controlled trials.”
Furthering that misleading impression, MacIntyre and Chughtai end their reply to Haslam by declaring that “a WHO-commissioned study has shown that masks reduce the risk of infection with beta-coronaviruses by 85%, and are equally protective in community and healthcare settings.” However, that WHO-commissioned study is not an RCT but an analysis of observational studies. Thus, it cannot prove that “masks reduce the risk” of anything. That is precisely why the authors of the study write that their results have “low certainty.”
Compounding the deceit, the CDC published a study in July 2020 that cites MacIntyre and Chughtai’s paper while claiming that they analyzed “randomized trials and concluded that use of face masks and respirators appeared to be protective in both health care and community settings.” Again, none of those findings are actually based on RCTs.
Beyond the CDC’s false portrayal of non-RCTs as RCTs, the same CDC study ignores the actual RCTs, all of which show no statically significant benefit from community masking. To reiterate, these studies are systematically analyzed in papers and reports published by:
- Emerging Infectious Diseases (the CDC’s own journal).
- the journal Epidemiology & Infection.
- the Center for Evidence-Based Medicine at Oxford University.
- the journal Influenza and Other Respiratory Viruses.
- the journal Clinical Infectious Diseases.
- the World Health Organization.
- the journal Annals of Internal Medicine.
The misinformation spread by MacIntyre, Chughtai, and the CDC cannot fool informed people with time to vet it, but it can muddle the issue enough to prevent all but the most tenacious researchers from finding the facts. Combined with the power of big tech corporations who suppress facts that contradict the CDC’s claims about masks, this is more than enough misinformation and censorship to keep the vast bulk of people in the dark.
In summary, a large array of gold-standard studies have found inconsistent benefits from higher-quality masks in healthcare settings and no statistically significant benefits from any type of mask in community settings. Crucially, the only RCT to evaluate cloth masks found that mandating them causes significant disease transmission in high-risk healthcare settings.
Faced with a mountain of RCTs that undercut their claims, proponents of community masking ignore or deceitfully dismiss them. For example, the CDC’s “Science Brief” on “Community Use of Cloth Masks” does not rely on a single RCT to support its claim that “universal masking” reduces the spread of C-19.
Instead, the CDC ignores all but two of the RCTs, which it brushes aside in a single paragraph. One of these is the lone RCT on cloth masks, and the manner in which the CDC tries to spin it is a textbook case of junk science:
- The CDC declares that the study was “unblinded,” which could bias “self-reporting of illness.” Blinding is a research technique in which people involved with a study don’t know who is receiving treatment (and who is not) so that they don’t react differently. The duplicity of the CDC’s criticism is exposed by the simple fact that all non-lab studies of masks are unblinded because the participants can easily tell if they are wearing a mask and what type of mask they are wearing. As the study states, “The laboratory results were blinded and laboratory testing was conducted in a blinded fashion,” but because “facemask use is a visible intervention, clinical end points could not be blinded.” Yet, the CDC misleads by singling out this one study as “unblinded,” even though this is the case with every real-life study of masks.
- The CDC alleges that the study is flawed because the participants created “the risk of infection” by handwashing and reusing their masks. That rationalization ignores the fact that people who use cloth masks in community settings also handwash and reuse their masks. Furthermore, each of the study participants was “provided with five masks,” told to wash them “with soap and water every day,” and “supplied with written instructions” on how to do this. If healthcare professionals in a clinical study became infected as a result of this protocol, why wouldn’t the general public?
- The CDC claims that the study suffers from “limited source control as hospitalized patients and staff were not masked.” Source control is using masks to prevent viruses from exiting (as opposed to entering) people’s mouths and noses. Contrary to the CDC’s complaint, the study was designed to address this issue by using a method called “cluster randomization.” This involves giving “the same treatment” (i.e., mask) to people who work together. The authors of the study explain that they used this method to find out if the “prevention of one infection in an individual can prevent a chain of subsequent transmission” to their coworkers. In addition, the study included a tightly controlled lab experiment on cloth masks which found that their “filtration was extremely poor” and 97% of all respiratory particles passed right through them. (More details about this are provided below in the section on laboratory studies.)
- The CDC argues that the study lacked “a true control (no mask) group for comparison.” That is a blatant half-truth because the CDC neglects to mention that people who were assigned to wear cloth masks were 3.49 times as likely to become infected than people who were assigned to “continue with their normal practices” of wearing masks occasionally. For the record, the study didn’t have a completely maskless group because a medical board “deemed it unethical to ask participants to not wear a mask.” Ironically, the results of the study suggest it is unethical to ask people to wear a cloth mask, which the study required of them.
- Finally, the CDC states, “A follow-up study in 2020 found that healthcare workers whose cloth masks were laundered by the hospital were protected equally as well as those that wore medical masks.” As evidenced by the coming facts, that statement epitomizes the adage, “If you torture the data enough, it will confess to anything.” Here again, MacIntyre and Chughtai are complicit:
- In June 2020, MacIntyre and Chughtai submitted a follow-up paper to their 2015 RCT on cloth masks (the same one that found mandating cloth masks amplifies disease transmission in high-risk healthcare settings).
- Their new 2020 paper was based on the same study as the original 2015 paper, which examined three measures of infection. Without explanation, however, the new paper failed to examine the only “statistically significant” measure of infection found by the original paper. Instead, the new paper only examined one of the measures that were “not statistically significant.” Just Facts asked MacIntyre why they made this baffling choice and has not received a reply.
- Only 22 people in the original study used “hospital laundry” as their sole method of washing, and the new paper does not report the infection rate for this group. Instead, it lumps them in with 91 people who used a combination of laundry and handwashing. Then it uses a statistical “technique” to supposedly determine whether infections among these people are counted in the laundry group or handwashing group.
- The new analysis suffers from a fatal flaw that a 2016 paper in the journal Nature calls one of the “most common” “invalidating errors” that plague peer-reviewed research: failing to incorporate the “number of clusters” (not just the number of individuals) into analyses of cluster randomization trials.
- Most simply and perhaps most importantly, the subjects in the study were not randomly assigned to wash their masks by hand or by hospital laundry. This means the new analysis is not an RCT. Yet, the authors included the words “analysis of a randomised controlled trial” in the title of their paper, giving the polar opposite impression.
Bottom line: the manner in which certain people disregard and twist gold-standard studies on masks says little about the studies but reveals a great deal about the people.
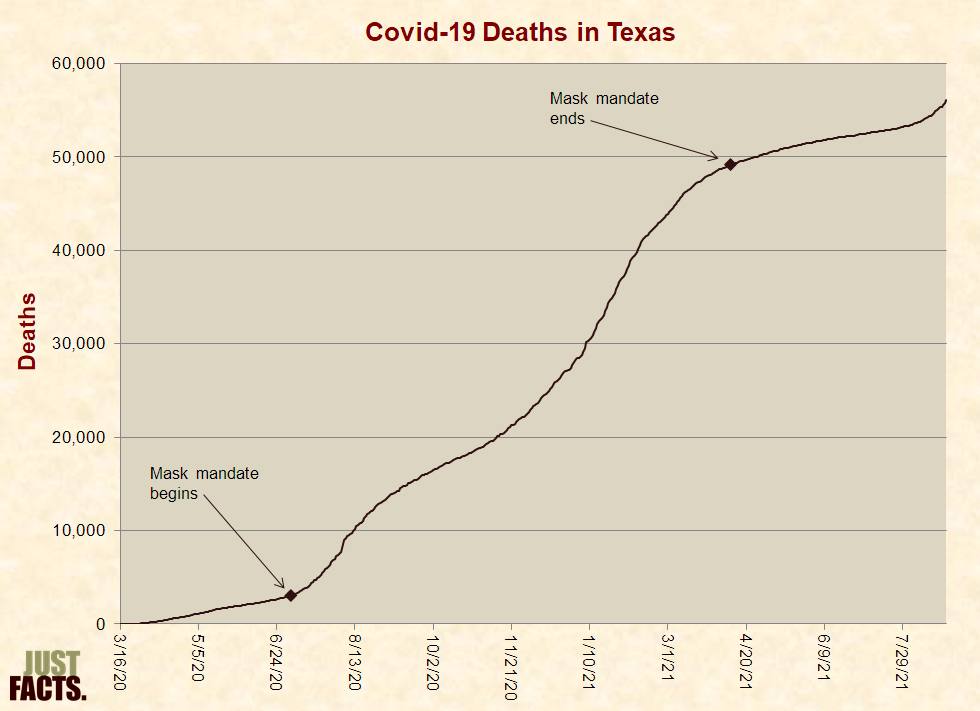
To repeat, observational studies cannot determine the effects of medical treatments except in rare cases. This is because many factors influence people’s health, and without an RCT, it is impossible to isolate the effects of any one factor from all of the others. A simple but vivid example that highlights this reality is the number of C-19 deaths in Texas before, during, and after its mask mandate: