The U.S. Centers for Disease Control and Prevention (CDC) is tracking multiple cases of monkeypox in the United States and other countries.
There were 15 confirmed cases in the United States in eight states, as of May 30, according to the CDC: three each in California and Florida, two each in Colorado, and New York, and one each in Massachusetts, Virginia, and Washington.
Monkeypox is an ancient viral disease that was largely confined to Africa in the past. It is thought to be endemic to certain rodent species.
Monkeypox Is Different
It is extremely unlikely monkeypox will trigger a pandemic because it is completely unlike COVID, stated Brenda Fitzgerald, a former director of the CDC, in an interview with The Daily Signal, on May 23.
“The problem with COVID-19 is that it was a new virus and you had to make some assumptions about what it would do and then act accordingly,” said Fitzgerald. “And we may not have done that correctly or … maybe did not evaluate correctly what to do. But this is a completely different business because this is a known virus…”
Public health officials gave conflicting messages on wearing masks and whether asymptomatic people could spread the coronavirus, says Fitzgerald.
“In my opinion, those comments should never have been made with an unknown disease,” said Fitzgerald.
Pet Prairie Dogs Carried Pox
This is not the first U.S. outbreak of monkeypox, which infected 47 people in the Midwest in 2003, says Fitzgerald.
“The important thing about [monkeypox] was that it was transferred in a way that we were well familiar with, in that they got it from animals,” said Fitzgerald. “In this particular case, they were prairie dogs that were being sold as pets.”
Monkeypox did not spread from human contact like cold viruses, says Fitzgerald.
“The most important thing is, nobody else gave it [to another person],” said Fitzgerald. “The person-to-person transmission for this virus is that you’re exposed to the lesions [and you have] prolonged face-to-face contact.”
‘DNA Viruses Mutate Very Slowly’
There are key differences between COVID-19 and monkeypox, Jane Orient, M.D., executive director of the Association of American Physicians and Surgeons, president of Physicians for Civil Defense, and a policy advisor to The Heartland Institute, which co-publishes Health Care News, wrote in an email to opinion leaders.
Unlike COVID-19, pox evolved over a long period, according to Robert Malone, M.D., a developer of mRNA technology, wrote Orient.
“The pox virus is a DNA virus,” said Orient. “Unlike RNA viruses, DNA viruses mutate very slowly. Monkeypox is similar to smallpox but far less lethal and less contagious.”
When smallpox cases became rare, the adverse effects of mass vaccination came to outweigh the risk of infection, says Orient.
“Routine smallpox vaccinations were discontinued in 1971, because of serious adverse effects, including myocarditis, and it is only available now for persons at high risk,” said Orient.
Sexually Transmitted?
The CDC is urging health care providers to look for patients with rashes, regardless of specific risk factors such as travel, gender, or sexual orientation, as signs of monkeypox.
Although monkeypox is not classified as a sexually transmitted disease (STD), that is the way the current outbreak has spread from Africa to developed countries, says Orient.
“There is no evidence of asymptomatic transmission of monkeypox, and all current cases in the West appear to be men having sex with men,” said Orient.
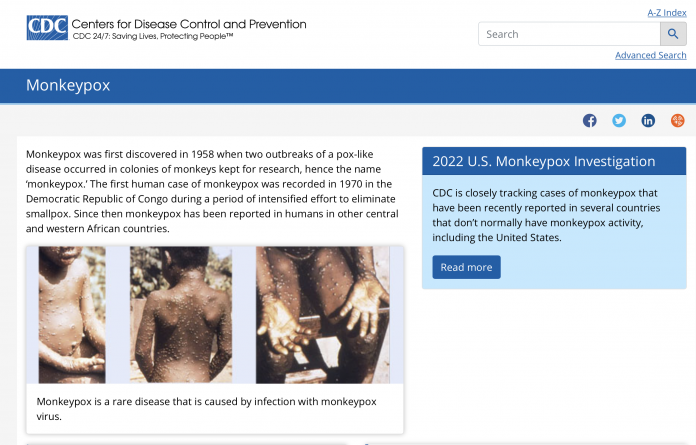
The physical signs of monkeypox are similar to other medical conditions, says Orient.
“The systemic symptoms of monkeypox—swollen lymph nodes, myalgia, asthenia, back pain, and headache—are also listed adverse effects of COVID-19 vaccines,” said Orient. “An image of a rash attributed to monkeypox appears to be a photograph of a shingles rash. Incidentally, shingles outbreaks have been reported after COVID vaccinations.”
Smallpox Vaccine Effective
The U.S. Food and Drug Administration (FDA) has approved the smallpox vaccine for use against monkeypox, and it is about 85 percent effective, but she advises against getting the shot if you did not receive the smallpox vaccine as a child, said Fitzgerald.
“If you are in that situation where you’re going to be a health care worker who’s taking care of people, a lot of people … then yes,” said Fitzgerald. “Obviously, there are special circumstances. But for the general population, no.”
Vaccines aren’t necessary to end this outbreak, says Orient.
“Monkeypox should be easily controlled by classic public health measures of isolating symptomatic individuals and temporary quarantine of those with close physical contact with an infected person,” said Orient.
People Control
The public should be on guard, says Matt Dean, a senior fellow for health care policy outreach at The Heartland Institute.
“People are easier to control when they are scared,” said Dean. “That this was used by governments around the world to increase and consolidate power during the COVID-19 pandemic now seems irrefutable.”
People are increasingly suspicious of the National Institute of Allergy and Infectious Diseases (NIAID) and its parent agency, the National Institutes of Health (NIH), says Dean.
“The distrust many Americans have for our own FDA, NIAID, or NIH because of the conflicting and obviously politically motivated guidance over the past 30 months rests on a growing body of evidence that suggests our fears and liberties were used against each other for the gain of others,” said Dean. “This sad fact shows how damaging it can be when politicians dictate the science of medicine.
Bonner R. Cohen, Ph.D. (bcohen@nationalcenter.org) is a senior fellow at the National Center for Public Policy Research.