Medicaid spending on children shifted sharply away from children in states that expanded the program under the Affordable Care Act to include able-bodied adults, a new study finds.
The Affordable Care Act’s Medicaid Expansion Is Shifting Resources Away from Low-Income Children, published by the Mercatus Center at George Mason University, also notes less than robust enrollment growth for the aged and the disabled in the expansion states.
“The expansion of Medicaid had the good intention of promoting health,” write study authors Charles Blahous and Liam Sigaud. “But well-intended policies can have unintended side effects.”
The study analyzed per capita expenditures for children and adults during Fiscal Years 2013 to 2019. The authors found Medicaid spending on low-income children in expansion states increased by 5.9 percent over the period, whereas in states that chose not to expand, the growth in spending on children was nearly three times higher, at 22.7 percent.
Expanded Demand
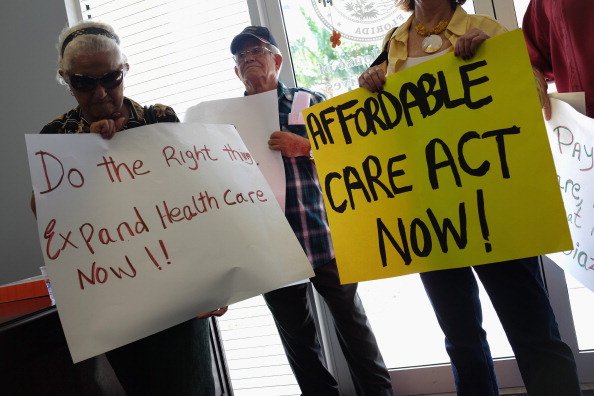
The Affordable Care Act, which went into effect on March 23, 2010, expanded health insurance coverage and required states to expand their Medicaid programs to include able-bodied adults with incomes up to 138 percent of the poverty level.
The U.S. Supreme Court later ruled the federal government could not force states to expand Medicaid, making the increases optional. According to the Kaiser Family Foundation, 39 states and the District of Columbia had expanded their programs as of November 9. In expansion states, nearly all adults earning up to $17,774 annually (for individuals) qualify for health care coverage at no cost to them.
Under expansion, Medicaid enrollment increased by 22 percent without an equal increase in health care providers. In addition, Medicaid pays physicians 54 percent of what they are reimbursed under private insurance, and hospitals receive 62 percent less than private insurers pay, which makes it less attractive to providers, write Blahous and Sigaud.
Unintended Consequences
As a result, families with low-income children in expansion states have more difficulty in finding physicians and getting timely appointments, Blahous told The Heartland Daily Podcast on January 9.
“A lot of children’s health is preventative: wellness checks, you do things to keep children on track; whereas spending for the disabled, the aged, a lot of that probably occurs on an emergency basis, and those people may wind up closer to the front of the pipeline more often,” said Blahous.
“Policymakers must understand how Medicaid’s financial resources are being shifted away from children as a byproduct of program expansion,” write Blahous and Sigaud. “When contemplating future Medicaid policy adjustments, they must consider how the opening of services to new enrollees affects the resources available to previously eligible enrollees. This is especially important in the case of low-income children, who are inherently vulnerable and for whom access to health services can have pronounced long-term effects.”
Unaffordable vs. Free
Medicaid expansion has created a host of distortions in the health care system, says Matt Dean, a senior fellow for health care policy outreach at The Heartland Institute, which co-publishes Health Care News. Dean saw the unintended consequences of expansion first-hand while serving seven terms in the Minnesota House of Representatives.
“While Minnesotans were paying more and more to get less and less health insurance, others were paying less and less to get more and more—a lot more,” said Dean.
Private health insurance is unaffordable for many working families in Minnesota, yet people from any state can get the best health care in Minnesota for free, says Dean.
“A farmer was paying $40,000 a year for family health insurance and was unable to obtain a policy at any price that would allow his family to go to the Mayo Clinic, which was a priority for him,” said Dean. “Meanwhile, anyone without income from any state can appear at Mayo and be treated for free, if they simply declare the intent to move to Minnesota, as they will be retroactively enrolled onto Medicaid.”
Free Riders
Another problem is ineligible people have been enrolled in Medicaid, says Dean.
“Minnesotans are asked to pay for folks who do not qualify for Medicaid because they may live in another state, make too much money, or are dead,” said Dean.
Medicaid-managed care plans do not check whether enrollees qualify, says Dean.
“I sponsored legislation that would ask Medicaid plans to directly contact the patient before they received payment for a Medicaid enrollee,” said Dean. “The ‘I’m Not a Robot’ bill would simply ask insurance companies to receive confirmation that a patient is alive, lives at an address, and wants coverage, before tax dollars are sent to the insurance company. Some patients no longer qualify, while others are covered by Medicaid with multiple plans, each receiving a check from the government to cover the patient.”
Individuals in need have been shoved aside, says Dean.
“States were given a financial incentive to essentially move newly eligible enrollees—who may have had private insurance—ahead of poor or disabled folks who may have no insurance,” said Dean.
AnneMarie Schieber (amschieber@heartland.org) is the managing editor of Health Care News.
Internet info:
Charles Blahous and Liam Sigaud, “The Affordable Care Act’s Medicaid Expansion is Shifting Resources Away from Low-Income Children,” Mercatus Center at George Mason University, December 13, 2022: https://www.mercatus.org/research/research-papers/affordable-care-acts-medicaid-expansion-shifting-resources-away-low-income
“Medicaid Expansion Moves Low-Income Children to the Back of the Line—Charles Blahous,”
The Heartland Daily Podcast, January 10, 2023: https://podcasts.apple.com/us/podcast/medicaid-expansion-moves-low-income-children-to-the/id557620400?i=1000593334283